Total Knee Replacement Surgery
A painful, stiff knee can keep you from doing the simple things in life, like walking without pain. Your physician may be able to replace your problem knee thanks to improved surgical techniques and materials. After a total knee replacement, you will have some restrictions when using your new knee, but you can look forward to returning to many activities of daily living.
History
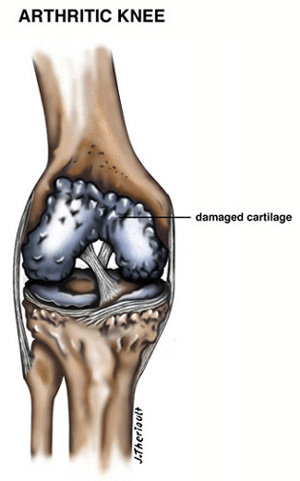
Chronic knee pain is commonly caused by arthritis. There are three common forms of arthritis: osteoarthritis, rheumatoid arthritis, and traumatic arthritis.
Osteoarthritis usually occurs in patients over 50 years old, and very often patients will have a family history of arthritis. The cartilage in the knee that acts as a cushion for the bones thins out and wears away. This, in turn, allows for the bones to rub together causing pain and stiffness.
Rheumatoid arthritis is a disease which there is thickening and inflammation of the synovial membrane. Over time, this chronic inflammation can cause cartilage damage, leading to pain and stiffness.
Traumatic arthritis can follow a serious knee injury. Fracture or ligamentous injuries may damage the articular cartilage over time, causing knee pain.
As your knee pain and stiffness increase, simply walking or climbing stairs can hurt. Conservative treatment is always attempted first. Anti-inflammatories, physiotherapy, activity modification, ambulatory assistive devices, braces, corticosteroid injections, and viscosupplementation are common conservative treatment options attempted before total knee replacement is considered.
Walking without pain is only possible when the bones in your knee joint are cushioned by healthy cartilage. You also need strong muscles and ligaments for stability, because your knee is more than a simple hinge joint. Each time you bend your knee to walk or climb stairs, the bones rotate, roll, and glide on each other.
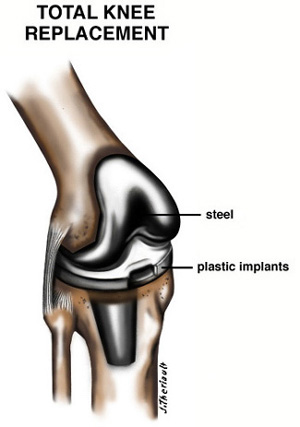
Like a normal knee, your prosthesis has smooth, weight-bearing surfaces. The femoral component covers your thigh bone, the tibial component covers the top of your shin bone, and the patellar component covers the underside of your kneecap. Your physician will choose the best prosthesis design, either cement or cementless, for your knee.
Your Orthopedic Evaluation
Your orthopedic evaluation helps your physician determine if you are a candidate for total knee replacement surgery, and if you are, to choose the best prosthesis for your particular knee problem.
Your medical history includes questions about knee pain, medication you may be taking, prior injury, infections, bleeding disorders, and other bone or joint problems you may have.
Your physical exam includes assessing your range of motion, any deformities in your legs (bowlegged or knock-kneed), stability, and watching how you walk and sit. X-rays will be taken to determine the extent of damage and deformity in your knee.
Deciding on Surgery
After your evaluation, our team will discuss whether total knee replacement surgery is the best treatment for you at this time. Your clinician may recommend some or all of the conservative treatment options mentioned above, or maybe even a different surgical procedure, such as a tibial osteotomy or an arthroscopy.
Understanding the risks and complications is part of your decision. Your physician will talk with you about infection, blood clots, stroke, heart attack, anesthetic problems, pneumonia, stiffness, pain, prosthesis loosening, blood vessel or nerve loss, or other post-operative risks before you decide on total knee replacement surgery (MAKE SURE YOU UNDERSTAND THESE RISKS).
Prior To Surgery
You will be asked to AVOID ASPIRIN, BLOOD THINNERS, OR ANTI-INFLAMMATORY MEDICATION FOR TWO (2) WEEKS PRIOR TO SURGERY TO MINIMIZE BLEEDING. You will also be asked to STOP SMOKING to decrease the chance of post-operative lung complications.
Continue leading a normal, healthy lifestyle, and be sure to let the doctor know about any infections or leg sores. You should call your doctors office if any medical problems arise that may require rescheduling of your surgery. Be particularly aware of any urinary problems such as burning, difficulty voiding, frequent urination, or other symptoms of infection, and report these immediately before your surgery.
It is VERY IMPORTANT to report any infection in your body before and after surgery. Any skin lesions in the area of your knee may cause a delay in surgery.
The morning of surgery, you will have an IV (intravenous) line started for medications before you are given general anesthesia. You can expect surgery to take from two to three hours, depending on how much damage to the knee has been sustained.
The Hospital Recovery Period
After surgery, you may wake up feeling a bit groggy. Specially-trained nurses will be with you to keep you comfortable and provide pain medications. Your nurses will also coach you with coughing and deep-breathing exercises to help clear your lungs and prevent post-operative complications. You will have a large dressing on your knee with a drain for normal post-operative bleeding. Once you are awake and alert, you will be transferred to your hospital room.
Once you are back in your room, the goal for the rest of your hospital stay is to begin walking again before you go home. You will be started on a physical therapy program to exercise you knee muscles and regain strength and range of motion in your new knee. These exercises will also improve circulation to your leg, improving the healing time.
Physical Therapy
Physical therapy, a vital part of the recovery, helps you regain your full knee potential. Gentle knee exercises strengthen the muscles around your new knee and help restore its range of motion. Your physical therapist will design a program especially for you, and teach you how to do rehabilitation exercises. Your therapist also starts you walking, a few steps at a time, to promote healing. Progressing from a walker to crutches, and finally a cane, helps you to regain confidence and your normal walking motion. This is hard work, and you must show perseverance and determination in doing your exercises if you want to get the best results possible.
Going Home
Once you have recovered and can bend your knee enough to go home, your surgeon will discharge you. Prior to your surgery, you may organize a short stay (1-2 weeks) at a skilled nursing facility. This will give you more time to work on rehabilitation to increase strength and range of motion in your knee. Your sutures and bandages are usually removed before you leave the hospital/skilled nursing facility, at which point you are given instructions for safe home recovery, which often includes follow-up physiotherapy. Feel free to ask any questions that you may have.
Your Home Recovery
At home, your goal is to return safely and comfortably to your activities of daily living. Your follow-up physiotherapy relieves any stiffness and awkwardness you may feel, and helps you regain independence as you learn to care for your new knee. Most patients return to normal activities 3-6 weeks following surgery. Night pain is common for several weeks after surgery. Driving can begin when your knee bends sufficiently enough to enter and sit comfortably in a car seat, and when your muscle control provides adequate reaction time to switch from accelerator to brake, which typically takes 4-6 weeks.
|
If at any time during your recovery, you notice fever, redness, increasing stiffness, calf pain, or shortness of breath, report to the emergency department IMMEDIATELY! |
Follow-up Physical Therapy
Your physical therapist will instruct you to continue with the exercises you learned in the hospital, and may teach you others as well. Strength exercises tone your thigh muscles, which have the greatest control over your new knee. Range of motion exercises help you bend and straighten your knee more fully.
Caring for Your New Knee
Your knee prosthesis is the result of years of research. Like any other device, your new knee’s life span depends on how you care for it. In your follow-up visits after surgery, your physician will follow your progress and answer any questions your may have about caring for your new knee.
Helpful Hints
- Follow your physician’s advice on using crutches or a cane to keep weight off your healing knee.
- Keep in mind that your prosthesis is designed for activities of daily living, not sports.
- Before dental work or surgery, let your doctor know you have a new knee; antibiotics may be needed to help prevent infection.
- If your prosthesis wears out or loosens, it can be replaced with another. Revision surgery is difficult, however, so preserve your new knee.
Enjoying Your New Knee
After a total knee replacement, you can look forward to less knee pain, stiffness, and deformity in your leg. While your new knee is not a normal knee, you can expect to enjoy your activities of daily living with greater ease and comfort. You can once again enjoy life with a more independent, mobile lifestyle.
There are limitations, however, and you will not be able to do all of the activities you did when your knee was healthy and normal. This is a major operation, and should only be done when all other treatments fail and pain persists.
|
BEFORE your surgery, make sure you understand all of the risks and complications, as well as possible alternative treatments. |
